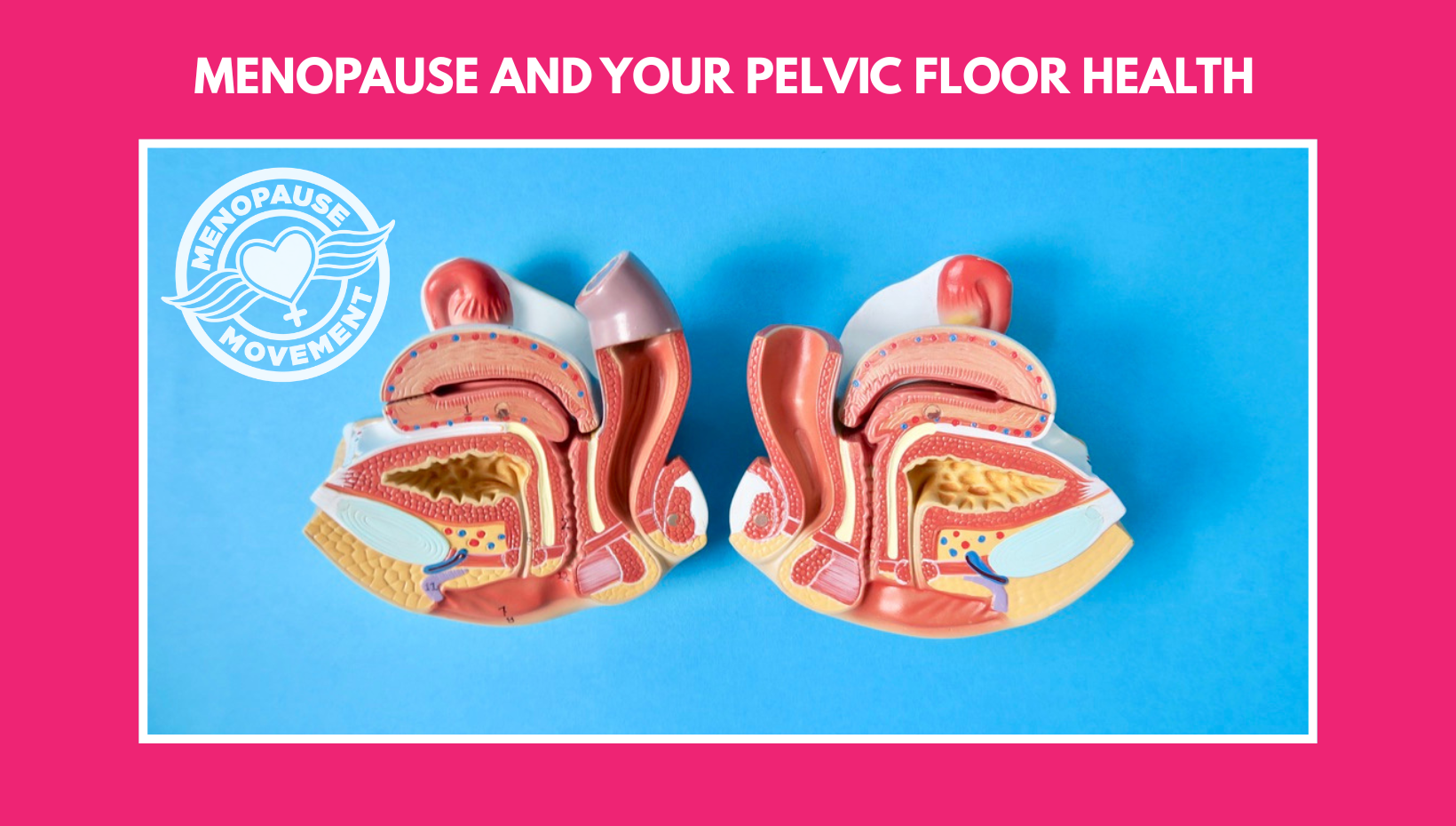
Pelvic health physio and co-founder of Menopause Movement, Christien Bird, sheds light on the impact of menopause on women's pelvic floor health, and the importance of pelvic floor training.
During perimenopause and menopause, declining oestrogen levels can significantly affect the pelvic floor. For many women, this contributes to bladder and bowel symptoms, pelvic discomfort, and changes in sexual function. These symptoms are common — but they are not inevitable, and they are certainly not something you need to “just live with.”
The pelvic floor is a highly responsive group of muscles that support the bladder, bowel and uterus. These muscles play a vital role in:
As oestrogen levels decline during menopause, changes occur not only in the pelvic floor muscles themselves, but also in the bladder, urethra and vaginal tissues. Reduced blood flow, thinning of tissues and loss of elasticity can all contribute to symptoms.
Common menopausal pelvic floor symptoms include:
While these symptoms affect over half of women at some point, effective treatments exist — and early intervention can make a profound difference.
To understand the pelvic floor a helpful analogy is the boat in a dock
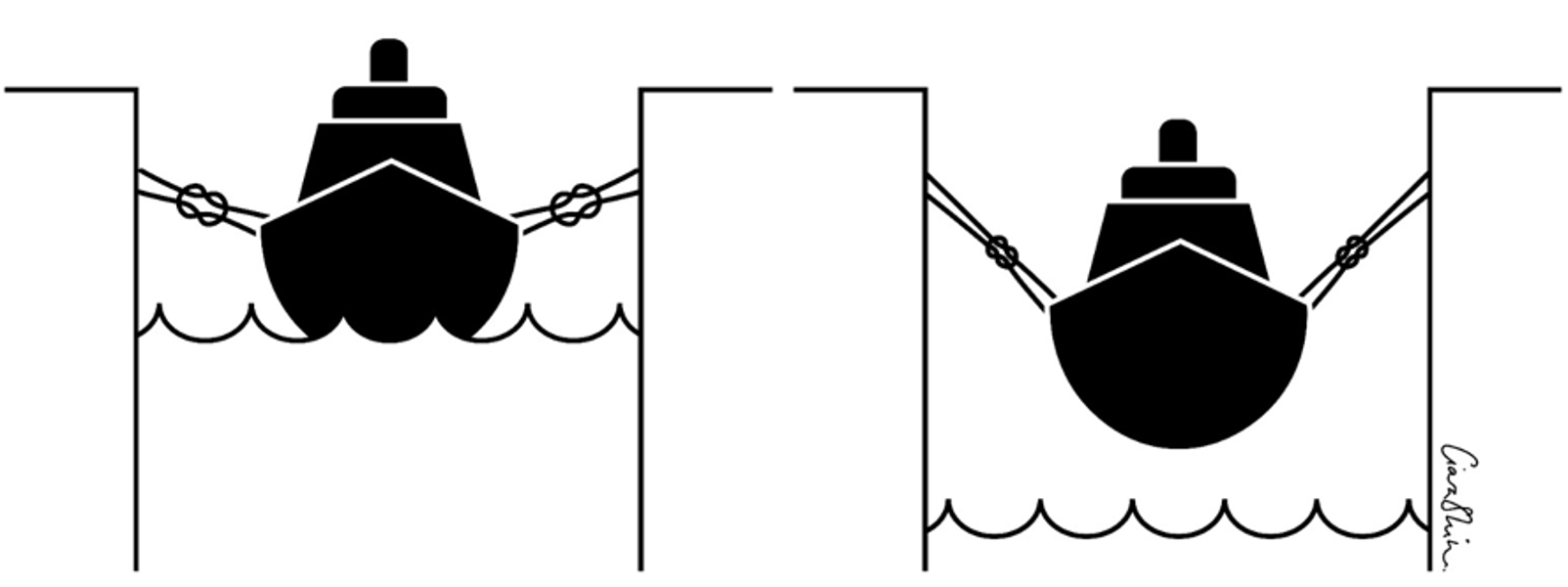
The ropes holding the boat to the dock are the ligaments and fascia support to supporting the organs above.
The water represents your pelvic floor muscles, absorbing the load.
If the water level drops, the boat drops down and puts strain on the ropes. If the water level rises, it takes the strain off the ropes. If the ligaments and connective tissue are overstretched from for instance childbirth, or changes into the MP, the PFM can help to compensate for this by supporting the pelvic organs. If PF muscle training is not enough to help prolapse or continence issues, there are other techniques and devices we can help women with, one example silicone pessaries, like a sports bra for the bladder neck and or vaginal walls. Most important is that you don’t give up and seek help.
There is strong medical evidence that pelvic floor muscle training (PFMT) is one of the most effective first-line treatments for urinary incontinence and pelvic organ prolapse — including in post-menopausal women.
A well-designed pelvic floor programme improves:
Importantly, clinical trials show it is never too late to start.
Menopause brings structural and biological changes:
These changes can contribute to bladder symptoms and recurrent discomfort. Vaginal oestrogen, alongside pelvic floor muscle training, is a safe and effective option for most women and is widely recommended by menopause and pelvic health specialists.
Hormones are only part of the picture. Large studies show that factors earlier in life —particularly vaginal birth — influence pelvic floor health decades later. Research demonstrates higher rates of urinary leakage in women who have had vaginal deliveries compared to caesarean sections, regardless of whether the caesarean was planned or emergency.
Lifestyle factors such as:
can also increase symptoms during menopause and are modifiable — making this a critical window for prevention and support.
Leakage is a major barrier to exercise, despite physical activity being essential for long-term health. Studies show women who exercise are three times more likely to experience urinary leakage, yet many stop exercising rather than seek help.
When women are given permission to talk about pelvic health, the response is often relief. Simple screening questions and early referral can be life changing.
Pelvic floor dysfunction is a common — and modifiable — barrier to staying active. If you answer yes to any of the questions below, a pelvic health assessment is recommended:
If any of these resonate, you are not alone — and help is available.
Christien Bird
January 2026